What is COPD?
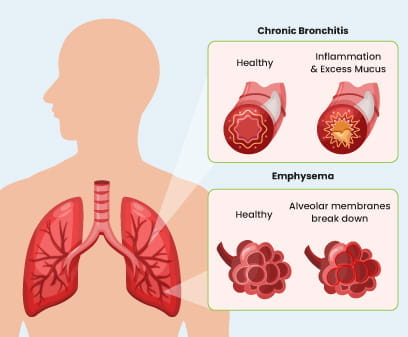
Chronic Obstructive Pulmonary Disease (COPD) is a lung disease that causes obstruction to the airflow leading to breathing problems. This condition can manifest as chronic bronchitis (inflamed and narrowed airways), emphysema (damaged air sacs), or both.
People with COPD have damaged lungs, which can get clogged by thick mucus known as phlegm. COPD is caused by exposure to harmful particles, like cigarette smoking, burning of biomass fuels, air pollution etc.
People with COPD are also at higher risk of other health-related problems such as pneumonia, heart failure, and increased anxiety.1
Types of COPD
Chronic bronchitis: If someone has a cough that produces mucus (phlegm) for at least three months in a row, and this happens for two years in a row, then this condition is known as chronic bronchitis.
Emphysema: It is a type of COPD in which air sacs in lung tissue lose their elasticity, leading to symptoms.2
Chronic bronchitis may coexist with emphysema, or patients may develop either condition independently.
Risk factors of COPD
Some activities can cause the airways to become narrow and lead to COPD.3

Smoking: Cigarette/bidi smoking is the leading cause of COPD. Ex-smoker can also have COPD

Passive smoking: Smoke being inhaled accidently from tobacco being smoked by others.

Household pollution: The smoke and pollutants emitted by chulhas can lead to chronic inflammation in the airways and lungs.

Workplace exposure: Breathing in chemicals, fumes, or dust at work can cause COPD.
COPD symptoms

Chronic cough: A persistent cough is common in people with COPD. It may produce mucus (sputum) that can be clear, white, yellow, green, or even blood-tinged.

Breathlessness: It may occur during physical activity and gradually worsen over time, even occurring during rest in advanced stages.

Wheezing: High-pitched whistling sound that occurs when breathing. It is caused by narrowed airways.

Tiredness: Due to the extra effort required to breathe, there can be fatigue and reduced stamina.

Chest tightness: Discomfort in the chest, which can worsen during physical activity.

Weight loss: Losing weight without trying (especially in later stages).

Recurrent Respiratory Infection: Getting sick with respiratory infections often.

Swelling: Swelling in the ankles, feet, or legs.
Diagnosis
To check your lungs and overall health, the following steps are taken by the doctor:
Medical history
Your doctor will ask you to provide details on the following questions to make the diagnosis:

Do you get breathless with exercise? Or when resting?

Do you cough up excessive sputum/mucus?

Do you smoke?

Have you had prolonged exposure to dust or air pollutants

Have you been coughing or wheezing for a long time?

Physical examination
Your doctor will do the following steps to examine you to help in the diagnosis of COPD:

Listen to the lungs and heart using a stethoscope.

Examine your nose and throat.

Check blood pressure, pulse and oxygen levels.

Check for swelling in feet and ankles.
Tests
Doctors use a simple test called spirometry to see how well your lungs work.
Spirometry measures the volume of air that can be inhaled and exhaled from the lungs.

Your doctor may also want to run a few other tests, such as:

Arterial blood gases (ABGs)
These tests are done to check your oxygen and carbon dioxide levels in the blood.

Chest X-ray or Chest CT scan
Imaging tests look for lung changes that COPD can cause.

Electrocardiogram (ECG or EKG)
This test checks your heart rhythm as a cause of breathlessness.

Exercise/walking testing
Your doctor might use this to find out if the oxygen level in your blood decreases when you exercise.
Grading COPD severity
COPD can get worse over time. How fast it progresses from mild to severe depends from person to person.4
COPD stages are classified based on spirometry test results which is generally conducted in a doctor’s clinic or hospital. These tests calculate FEV1 and FVC values.
Forced expiratory volume in one second (FEV1): This refers to the volume of air you can exhale in one second after a position of full inspiration. With healthy lungs and airways, you can typically blow out most of the air from your lungs within that time.
Forced Vital Capacity (FVC): It refers to the total volume of air you can exhale in a single breath after a position of full inspiration.
COPD is diagnosed if your FEV1/FVC ratio is < 70%, post the administration of an inhaler containing a bronchodilator drug. Your doctor will then grade your COPD into one of four stages—Mild, Moderate, Severe, and Very Severe—based on how much your FEV1 score is reduced for your age:

FEV1/FVC ratio < 70% FEV1 ≥ 80%

Grade 2: Moderate
FEV1 /FVC ratio < 70% FEV1 50% to < 80% of predicted value

Grade 3: Severe
FEV1 /FVC ratio < 70% FEV1 30% to < 50% of predicted value

Grade 4: Very Severe
FEV1 /FVC ratio < 70% FEV1 < 30% of predicted value4,7,8
COPD treatment
The treatment for COPD mainly focuses on relieving symptoms, such as coughing and breathing problems and avoiding secondary respiratory infections. Your doctor may recommend:
Bronchodilators:
These medicines help relax airways. To help breathe easier, bronchodilators are inhaled using an inhaler.
Anti-inflammatory medications:
These are steroids which can be taken by inhalers.
Antibiotics:
There can be further damage to your weakened lungs because of the frequent infections. To treat a bacterial infection, antibiotics might be needed on the advice of your doctor.
Supplemental oxygen:
If your blood oxygen level is low (hypoxemia), you may need a portable oxygen tank to improve your oxygen levels as per your physician's recommendation.
Expectorants:
These products help thin the mucus so that you can cough it out more easily.
Rehabilitation:
Pulmonary rehabilitation programs can help by teaching effective breathing techniques to reduce shortness of breath, enhance the overall quality of life, and improve the ability to exercise and perform daily tasks.
Vaccination:
Getting vaccinations to prevent flu and pneumonia is very important. Respiratory infections are more dangerous when you have COPD.4
Preventive measures of COPD progression
There are certain ways to slow down the progression of COPD.
The following steps can help you prevent the complications associated with COPD4,6:

Eat a healthy diet and stay physically active

Talk to your doctor if you are experiencing depression

Enrol in smoking cessation programs

Consult doctors for protective measures against occupational dust or chemical exposure

Avoid exposure to smoke or stop smoking
COPD complications
COPD often occurs alongside other diseases, which can make it worse.
Common heart-related issues in people with COPD include:

Heart failure

Coronary artery disease (narrowing of the blood vessels supplying the heart)

Irregular heartbeats

High blood pressure

Lung cancer and bronchiectasis (damage to the airways) are also common in COPD patients.

Osteoporosis (weak bones) and mental health issues like depression and anxiety are frequent but often not diagnosed, leading to worse health outcomes.

Acid reflux (GERD) can increase the chances of COPD flare-ups and worsen overall health.
Other issues include

Obstructive sleep apnea (breathing problems during sleep)

Insomnia (trouble sleeping)

Gum disease and poor dental health

Metabolic syndrome (a cluster of conditions that increase heart disease risk)

Diabetes

Anemia (low red blood cell count)
Reference
- Zabel P. Chronic obstructive pulmonary disease (COPD). Internist (Berl) [Internet]. 2006 [cited 2024 Feb 12];47(9):883–4. Available from: Click here
- Symptoms [Internet]. NHLBI, NIH. [cited 2024 Mar 19]. Available from: Click here
- Kamal R, Srivastava AK, Kesavachandran CN. Meta-analysis approach to study the prevalence of chronic obstructive pulmonary disease among current, former and non-smokers. Toxicology Reports. 2015;2:1064–74 (4)
- 2024 REPORT Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease [Internet]. 2024. Available from: Click here
- Meseeha M, Attia M. Alpha 1 Antitrypsin Deficiency [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2023. Available from:Click here
- Learn About Alpha-1 Antitrypsin Deficiency [Internet]. www.lung.org. Available from: Click here
- Dr Colin Tidy. Spirometry [Internet]. Patient.info. 2016. Available from: Click here
- Four stages of COPD [Internet]. Global Allergy & Airways Patient Platform. 2023. Available from: Click here
- Chapter 5: COPD and comorbidities. GOLD 2024 guidelines. [Internet]. 2024. [Cited 2024 June 12] Available from: Click here
- Dr Mary Harding. Chronic Obstructive Pulmonary Disease (COPD) [Internet]. Patient.info. 2018. Available from: Click here
- Living with Chronic Obstructive Pulmonary Disease (COPD) [Internet]. NHS. 2020. Available from: Click here
